For complex Endometriosis and Adenomyosis care, visit LotusEndo.com
Gynecologic Oncology Institute is no longer accepting new general gynecologic oncology patients, and refocusing on endo & adeno advanced treatment.
Pioneering the Future of Surgical Ovarian Cancer Care: Minimally Invasive Surgery
Accelerated Healing with Surgical Robotic Ovarian Cancer Diagnosis, Staging and Cytoreduction
Ovarian Cancer
Ovarian cancer, mainly endometriosis-related, is the focal malignancy Dr. Steve Vasilev and his team actively treat at our Gynecologic Oncology center in Los Angeles. Whether you are newly diagnosed with cancer of the ovary, considering treatment options for ovarian cancer, or seeking a second opinion, we work with you to provide a unique integrative surgical treatment plan that fits your individual situation and holistic needs. This includes minimally invasive robotic surgery whenever possible, even for advanced ovarian cancer stages, which is NOT available at most centers. We combine high-tech care with a personal touch, including holistic natural support. This includes proactive ovarian cancer-fighting lifestyle guidance and nutritional support counseling for every person.

Personalized High-Tech Ovarian Cancer Care
Ovarian cancer is highly variable, so you should seek personalized treatment options. Just like cancers differ, so do individual people and their specific situation. Dr. Steven Vasilev, Gynecologic Oncologist, recommended treatment options are based on how early your ovarian cancer is, the most likely effective treatments, and managing side effects. Most important are individual needs not only to survive but also to thrive.

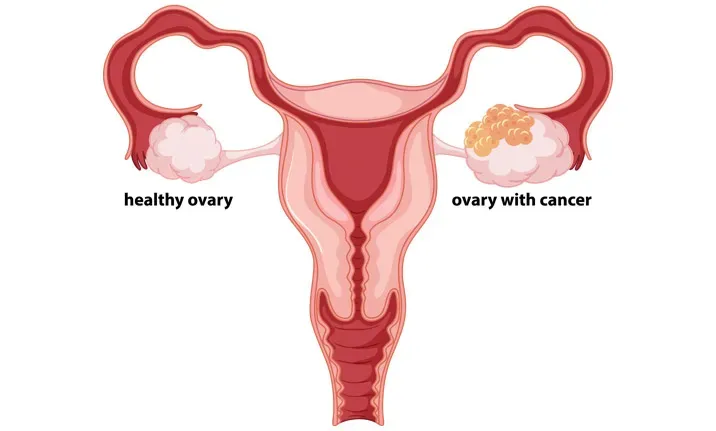
About Ovarian Cancer
Ovarian cancer, not surprisingly, arises in the ovary and can be inherited genetic (20%) or sporadic (80%). Endometriosis can increase your risk by up to 20X. Bad genes may increase your predisposition to developing cancer of the ovary so testing for genetic mutations like BRCA and many others is important if you have a family history of ovarian or breast cancer. However, even with an increased predisposition paying attention to environmental triggers (e.g. bad diet) and general health can reduce your risk.
-
Epithelial
-
Germ cell
-
Stromal
Major Types of Ovarian Cancer
Ovarian cancer is the second most common gynecologic cancer in the United States, as reported by national cancer institutes. Epithelial ovarian cancer, arising from the surface of the ovary, is the most common type (90%) and most commonly occurs in older women. Epithelial ovarian sub-types are further divided into serous, mucinous, endometrioid, clear cell, transitional and undifferentiated types. Less common types are germ cell (cells that make up individual eggs, occur in younger women, about 5% of ovarian malignancies). The main sub-types are teratoma, dysgerminoma, endodermal sinus tumor and choriocarcinoma. Stromal cells (cells that produce estrogen and progesterone, uncommon) are typically found in older women, but sometimes occur in girls. These sub-types include granulosa, granulosa-theca and Sertoli-Leydig cell tumors; which often do not spread as fast as other ovarian tumors, but can behave aggressively.
Late Stage Diagnosis Common
Ovarian cancer often goes undiagnosed for a long time because active symptoms are often overlooked or mistaken for common illnesses. Signs and symptoms include pelvic pressure, urinary frequency, constipation, bloating or sudden weight loss, loss of appetite, unusual fatigue, back pain, pain during sex, menstrual changes, pelvic or abdominal pain, indigestion or feeling full quickly, or abnormal or post-menopausal bleeding. Most of the time these symptoms are not related to ovarian cancer, but if you have them and they are worsening it is prudent to have your doctor evaluate you.


Ovarian Cancer Diagnosis
The only way to be certain of a diagnosis using today’s technology is tissue analysis or biopsy via surgery. Biopsy of the ovary with a needle passed through the skin is highly discouraged because if the diagnosis is cancer the needle can spill cancer cells and change the stage of the ovarian cancer. On the other hand, if there is some fluid outside of the ovary in the pelvis a needle aspiration under ultrasound or CT guidance (called cytologic analysis) can give the pathologist enough to make a diagnosis in many cases. Also, if a CT scan shows a lot of tumors in multiple places in the abdomen a needle biopsy of one of those is reasonable because this means the ovarian cancer is already spread and a biopsy will not change the stage.
In this case, the biopsy will simply help determine if it is ovarian cancer or some other type of cancer such as intestinal. The treatment plans are very different, so this is a reasonable thing to do before planning therapy. Pelvic ultrasound may be used to suggest if an ovarian mass looks benign or if its appearance is suspicious for ovarian malignancy. However, it is not diagnostic just on the basis of how an ovarian mass or ovarian cyst looks.
To determine if or how far the ovarian cancer may have spread, a MRI, CT scan or PET-CT scan may be used. Most often cancer of the ovary stays confined to the pelvic and abdominal area for a long time, rather than spreading to the lungs, liver, bones or brain. Having said that, it can produce fluid around the lungs and may erode into organ like the liver. So, a MRI, CT or PET-CT is usually ordered to look at all areas, including the chest, abdomen and pelvis. The results of these scans can help plan treatment for ovarian cancer.
Ovarian Cancer Biomarkers
Even though the CA-125 blood test is discouraged for screening, if cancer is strongly suspected or is confirmed by biopsy, this tests acts like a tumor marker. This may help firm up a diagnosis (other tumor markers exist for other cancers) and help determine how well treatment is working by monitoring CA-125 levels. Other tumor markers for epithelial ovarian cancers include CEA and HE4.
The OVA1 and OVERA panel of tests examines a combination of markers and can also be useful. Germ cell and stromal ovarian cancers have other biomarkers such as hCG, AFP, LDH and Inhibin. Newer molecular markers based on gene mutations are on the horizon and some are already offered today, albeit they are no standard of practice because research data regarding how to use these new markers is still in development.
Ovarian Cancer Treatment
Treatment of ovarian cancer strongly depends on the “stage”. Is the cancer still confined to the ovary or has it spread to other areas like the lymph nodes or organs? Staging cancer of the ovary includes information from a physical examination, basic X-rays and surgical findings. In addition, advanced radiologic tests like CT scans and PET scans are used to help determine treatment, but in the end the surgery is what determine ovarian cancer stage. The only exception to that is if any fluid or tumors in the lung area or inside the liver or spleen are proven to contain cancer cells using a needle biopsy. That means the ovarian cancer is in Stage IV.

Ovary Cancer Stages:
Stage I
Cancer is confined to the ovary.
Stage II
Cancer is present in the ovary and surrounding pelvic structures
Stage III
Cancer has moved out of the pelvis and into the abdomen or lymph nodes Stage
Stage IV
Cancer has spread to other organs like the lung area or is found within the liver or spleen
Primary Treatment Options for Cancer of the Ovary
Each of the above stages is sub-staged based on other factors like size of tumors and more. The ovarian cancer staging system is fairly complex and treatment is based at least partly on the stage, as well as the cell type (e.g. epithelial or germ cell) and other factors. Treatment is often, but not always, a combination of surgery and chemotherapy. For early-stage ovarian cancer sometimes surgery is all you need and, if fertility is desired during reproductive years, it may be possible to preserve the other ovary, tube, and uterus. However, the more advanced the cancer is the more likely that both ovaries, tubes, uterus, cervix and other tissues like lymph nodes and even parts of intestine will have to be removed to eliminate as much cancer as possible surgically.

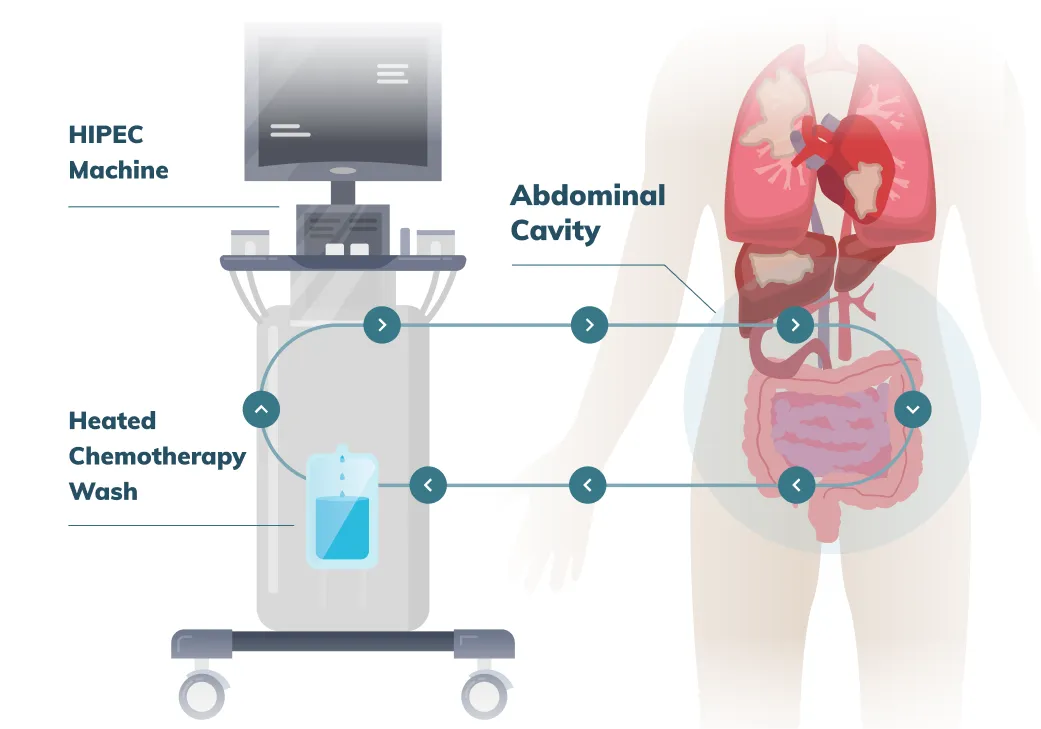
Surgery : Debulking or Cytoreduction
Ovarian cancer advanced surgery is called “debulking” or “cytoreduction” and is a key component of treatment. Traditionally it is performed using a very long incision from the symphysis (pubic bone) to the xiphoid (middle part of your ribcage) and this is often the standard of care in many hospitals. In a relatively few select centers around the world where highly specialized surgical expertise is available, like with us and Dr. Steven Vasilev MD, advanced ovarian cancer surgery may be possible using robotically assisted minimally invasive surgery through small incisions.
The recovery time is vastly improved, which allows getting back to life or to the next phase of treatment (chemotherapy) much quicker. Often recovery is also enhanced because the radicality of surgery (e.g. bowel resection) is reduced when the treatment starts with chemotherapy (roughly 3-4 times) followed by robotic surgery. After the surgery, several (2-4) more treatments with chemotherapy completes the plan.
Active Treatment for Recurrence
Even advanced ovarian cancer can be cured because it is very sensitive to the multiple types of chemotherapy we have available today. However, both in primary treatment, as well as treatment of recurrence the developing standard, uses molecular analysis (NGS or next-generation sequencing) to find options for very targeted biological therapies. The future is now and we are already using these. Sooner than later molecular targeted biologicals will replace standard chemotherapy which is not very targeted, killing normal cells as well as ovarian cancer cells.


Ovarian Cancer National Survival Rates
According to the American Cancer Society, the survival rates for ovarian cancer by stage on average are: For stage I ovarian cancer, the 5-year survival rate ranges from 75-95% For stage II ovarian cancer, the 5-year survival rate ranges from 65-80% The 5-year survival rate for stage III ovarian cancer ranges from 28-63% Stage IV ovarian cancer has a 5-year survival rate of almost 20% These numbers vary due to the sub-stages within each stage. Keep in mind that these are averages and there are always survivors in each stage category.
Ovarian Cancer Outcomes
Ovarian cancer survival rates are only estimates and there are survivors of any stage of any cancer, including survivors of advanced ovarian cancer.
Dr. Vasilev has personally led patients with advanced stage ovarian cancer to thriving in survivorship, ten, fifteen and more years after diagnosis.

There is no question that ovarian cancer has to be highly individualized and that is what we specialize in at the Gynecologic Oncology Institute. From very special and unique expertise in minimally invasive robotic cancer for the most advanced ovarian cancer to molecular analysis and targeted therapies, our approach is among the best you can find anywhere.
Robotic Ovarian Cancer Cytoreduction Outcomes
Regarding the surgical expertise and outcomes with robotic surgery, from early to advanced ovarian cancer, we stand nearly alone on the West coast. The following information is critical to consider. Ovarian Robotic Surgery Basic robotic training and expertise in pelvic surgery is becoming more common for uterine and cervical cancer. However, currently, radical robotic multi-quadrant ovarian cancer cytoreduction is not standard of care because an advanced skill set for this is not sufficiently prevalent among the majority of gynecologic oncologists. These are our published results for Ovarian Cancer Robotic Cytoreduction.

This expertise is slowly evolving with a relative handful of committed surgeons practicing nationally with adequate experience, who embrace the technique with strategies and tools to minimize the risk of conversion to laparotomy while achieving as close to “complete” R0 or CC0 cytoreduction as possible. Encouraging results have been published and mirror our success with minimally invasive ovarian cancer cytoreduction, mainly using robotic surgery due to the complexity of the surgery.

Minimally Invasive Surgery Outcomes
Our surgical experience with complex and re-operative robotics spans over eight years and thus far, for ovarian cancer cytoreduction, the results include low conversion rate of <1% with a high rate of complete CC0 macro-cytoreduction and practically all achieving more than "optimal" cytoreduction status with minimal CC-1 disease (a few millimeters or less = tiny rice kernel size or less). This is consistent with published results by other surgical groups as well as ours.
In selecting your surgeon it is critically important to understand the following. While today’s imaging with CT and PET-CT is good, it is not perfect to predict the extent of disease or distribution initially or after neo-adjuvant chemotherapy. Therefore, the potential carcinomatosis distribution is pan-abdominal and pan-pelvic. Literally, ALL eventualities need to be anticipated and prepared for to optimize outcomes with the lowest possible morbidity, lowest conversion rates to a big incision and to best achievable cytoreduction rates.
We have the specialized tools and advanced expertise to provide a very unique surgical benefit to you even in very advanced cancer situations. As noted, we are not alone nationally but stand in a very unique position regarding the ability to provide minimally invasive surgical options, even in the face of advanced disease.
Ovarian Cancer Survivorship Care
Beyond surviving ovarian cancer there is quality of life, which can be equally as important. This is especially true because ovarian cancer treatment can extend for a long period of time. To achieve the best quality of life after a diagnosis of ovarian cancer, a personalized treatment plan is crucial to beat your cancer and thrive. In addition, the treatment plan must evolve as time goes on. By focusing on you as an individual, and not just on your cancer, we guide you every step of the way. We specialize in helping you plan out the best outcomes possible based not just on your cancer but also on your body, mind, and spirit.

Critical Tips
-
Active Prevention is possible
-
Risk-reducing surgery
-
Earlier diagnosis
-
Cure is the goal
-
Minimally invasive robotic surgery
-
Proactive thriving survivorship
You can prevent cancer of the ovaries and possibly reduce the risk of ovarian cancer recurrence through integrative epigenetics and nutrigenomics.
If you are at increased risk for ovarian malignancy based on genetic assessment, you may strongly benefit from risk-reducing minimally invasive surgery to prevent ovarian cancer.
Stage I ovarian cancer is highly curable. Stage IIIc is the usual advanced diagnosis, and cure rates drop. Pay attention to unusual symptoms in your abdomen and pelvis.
Even for advanced ovarian cancer, combined surgery and chemo-biological therapies are increasing cures. Many options exist in today’s world of molecular assessment genomically targeted agents and immunomodulation.
Surgery + Medical + Integrative Rx
A strong combination plan is needed to get the best results and highest chance for cure and thriving.
Large incisions are a thing of the past in the hands of Dr. Steven Vasilev MD for the majority of patients. We are unique, amongst a relative handful across the country, with a very advanced robotic surgery skill-set for multi-quadrant ovarian cancer debulking or cytoreduction, even in advanced-stage disease.
What happens AFTER ovarian cancer treatment and surgery is……EVERYTHING !! This is where you engage in proactive survivorship with integrative nutritional, exercise and lifestyle modification for the best shot at recurrence risk reduction.
Review Ovarian Cancer FAQs
© Steven Vasilev MD | Gynecologic Oncology. All Rights Reserved 2015-2025.