For complex Endometriosis and Adenomyosis care, visit LotusEndo.com
Gynecologic Oncology Institute is no longer accepting new general gynecologic oncology patients, and refocusing on endo & adeno advanced treatment.
Conquer Endometriosis: Advanced Robotic Surgery and Integrative Holistic Healing
Empowering Your Journey to Thrive
Endometriosis Treatment
Dr. Steve Vasilev : An internationally recognized master robotic surgeon and endometriosis specialist focusing on endometriosis excision surgery and related malignancies. Experience a personal touch with holistic natural support that includes proactive lifestyle guidance and nutritional counseling for your unique needs.

About Endometriosis
Common but Under-diagnosed: Affects up to 1 in 10 women, with pain, bowel symptoms and infertility, yet diagnosis often delayed by many years.
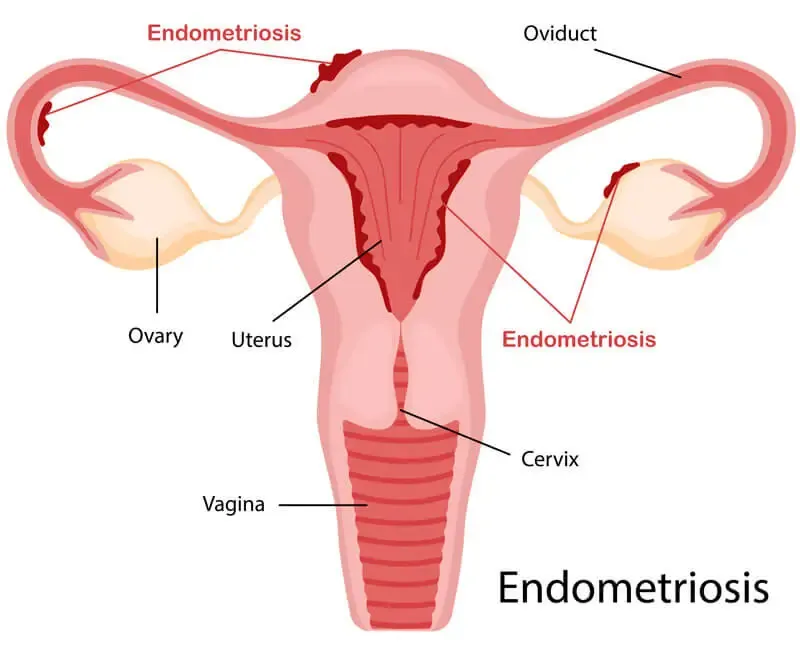
Misplaced Tissue: Occurs when cells similar to the uterine lining (endometrium) grow outside the uterus in the pelvis or abdomen.
Biological Differences: Implant cells differ significantly at the molecular level from normal uterine lining cells.
Today's Treatment: Advanced excision surgery, targeted hormonal therapies, integrative pain management and treatment options
Research Opportunity: Molecular differences offer potential targets for diagnosis and treatment being researched world-wide, including Dr. Vasilev's team at the SJCI laboratory.
Endometriosis Causes
Exact cause(s) unknown: Most likely multiple genes and multiple factors involved, including environment, hormones, immune and developmental or embryologic influences.
Major Subtypes
-
Superficial endometriosis (on surface)
-
Deep Infiltrating endometriosis (invading normal tissues & organs)
-
Ovarian endometriosis (endometrioma)
-
Metastatic endometriosis (benign spread to other areas) and Malignant Degeneration (1%)
Endometriosis can affect not only your pelvic organs and delicate structures, which include your bladder, ureters and rectum, but also outside your pelvis higher up in the abdomen. There it can involve your intestines. Endometriosis can spread literally anywhere in your body, including the lungs (metastatic) and beyond.

Endometriosis Prevention and Detection
While the near future may bring molecular genetic insights into targeted prevention, today there is no reliable way to prevent endometriosis. In fact, there is a genetic predisposition which is not well understood. If you have a relative with endo, you have a 5-7x risk of being affected. What those genetic switches are will be uncovered soon and prevention and treatment will be enhanced. Meanwhile, you can do a lot towards reducing the chances it will affect you and maybe decrease endometriosis progression. The following are integrative insights into endometriosis reducing lifestyle modifications and is as natural a strategy for endometriosis treatment as possible.
Regular Exercise
Through regular intensive workouts, you’ll be able to “whip yourself into shape” and most importantly, get to a low percentage of body fat (low BMI or body mass index). By reducing the amount of body fat less estrogen is made in those fat cells and you reduce the total amount of estrogen circulating in your body. Since estrogen feeds endometriosis, the less estrogen circulating in your body, within physiologic normal limits, the better. To emphasize, the best exercise for this is high-intensity interval training (HIIT) or “burst training”. Ideally, you should work with a personal trainer or someone in the gym for safety, but you basically want to go all out for 30 seconds and then rest for 90 seconds and then repeat over and over. This type of exercise builds muscle, which burns more calories from your diet and increases human growth hormone (HGH).

Whole Food Plant Based Diet
By eating lots of vegetables as the “base” of your diet, rather than sugar and relative junk, you will lose weight and reduce the estrogen in your body through less fat production as well as helping you maintain regular cycles. When your cycles are regular there is less chance that your body is in estrogen overload. The best animal protein is wild-caught fish like salmon. Maintaining healthy fiber in your diet also helps bind and flush excess estrogen.
In this video actress Tia Mowry explains endometriosis, and how dietary changes helped her. You should consider all of this in your overall treatment and prevention strategy.
Reduce Alcohol
Unfortunately, alcohol causes estrogen spikes in your body.
So, limit the drinking.
This is also a good cancer prevention strategy over the long run.


Reduce Caffeine
Simlar to alcohol, consuming a lot of caffeinated drinks per day (more than one) can cause estrogen levels to rise.
So, limit this or look for less caffeinated solutions like some teas.
Avoid Xenoestrogens
We are exposed to more than 30,000 toxins per year. Some of these can act as estrogens on your body and disrupt normal hormone function.
Sources include commercially raised meat and dairy products (especially processed meats), products with insecticide or pesticide residue, unfiltered tap water, many food additives and personal items such as conditioners, lotions, shampoos, soaps and even toothpastes.


Avoid Soy
This is controversial and, GMO arguments aside, the plant estrogens in soy can theoretically stimulate endo growth. Generally, you would have to consume gallons of it, but at least limiting soy products may help reduce total estrogen in your body.
The scientific counter-argument to this is that plant estrogens stimulate another part of the estrogen receptor on normal and abnormal cells (cancer or endometriosis) and may actually BLOCK the effect of regular estrogen. So the jury is still out on this concept and there may be a mixed effect.
Consume Seaweed
This is not proven but also has VERY little downside. Seaweeds, like bladderwrack, may have anti-cancer properties, including anti-estrogen effects.
Japanese women have among the lowest rates of breast, endometrial, and ovarian cancers, as well as longer menstrual cycles and lower estrogen levels circulating in their blood. Small animal studies and case reports in women suggest that this may alleviate some endometriosis pain due to a reduction of circulating estrogen levels.

Endometriosis Diagnosis

Diagnostic Scans and Biopsies
Imaging scans (Ultrasound, CT, MRI) are normal too often unless there is a pelvic mass which can possibly be an endometrioma. This is one of the reasons that diagnosis in the United States can be delayed by many years, if not decades, after the onset of symptoms. If you have persistent pelvic pain with normal scans, it is possible that you have endometriosis. The physical examination and detailed history of pain and overall assessment is important in helping determine if surgery should be performed for a diagnosis by biopsy.
Excision (biopsy) of an implant during minimally invasive surgery is the only way to make a certain diagnosis of endometriosis. Rarely, a needle biopsy guided by ultrasound or CT scan can make the diagnosis. The reason it is rare is that a needle is very small and even if you place the needle accurately in an abnormal area seen on imaging the amount of biopsy tissue is tiny. The pathologist may simply find inflammation and fibrosis or scarring and no active endometriosis. This does not mean it is not there and was only millimeters away from the area the needle biopsied.
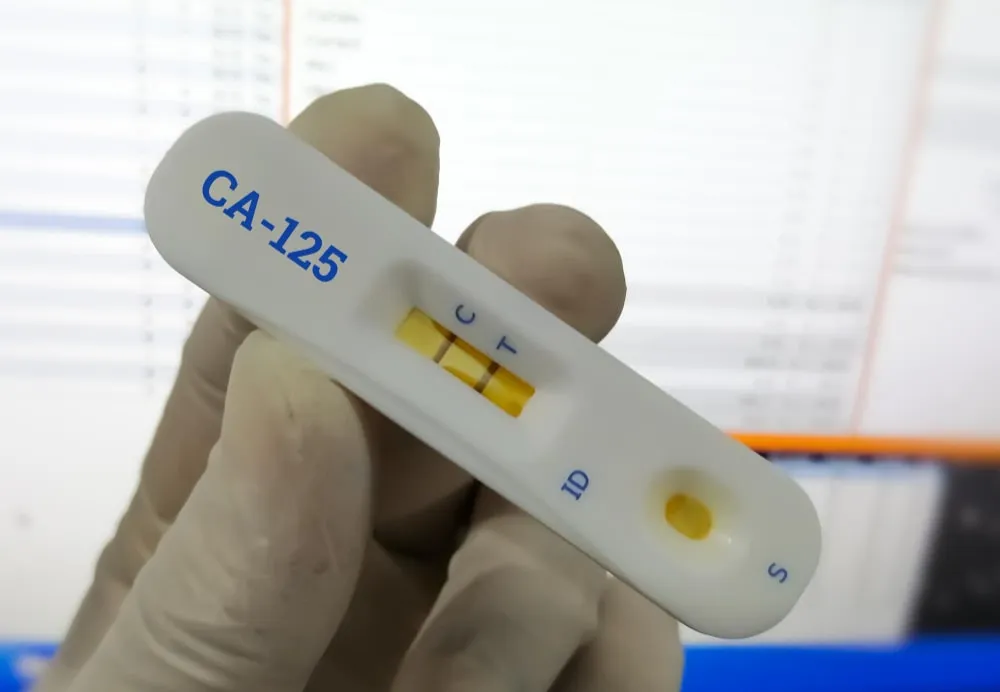
Endometriosis Biomarkers
Some blood tests, like the CA-125 “ovarian cancer tumor marker”, or CA19-9 may be elevated in endo.
This does NOT mean you have cancer because CA-125 and CA19-9 can be elevated in any inflammatory disease. Endometriosis is inflammatory.
With the advent of “omics”, including genomics, metabolomics, proteomics and other research areas, promising blood tests are being developed.
So far, none are accurate enough to help in the diagnosis or follow-up testing of endometriosis.

Endometriosis Treatment
Treatment of endometriosis is partly dependent on where it is located (pelvis or outside the pelvis) and what the stage is. Staging is a classificiation of the severity of pelvic endo.
Stages of Endometriosis
According to ASRM (American Society of Reproductive Medicine), there are four stages of pelvic endometriosis. This does not always correlate with the symptoms. Someone can have high stage and less pain than another person with lower stage and more pain. But this staging helps determine treatment and the type of surgery that might be best for you. The following is simplified but the general groupings are as listed.
-
Stage I or minimal endometriosis:
There are small patches or implants either on or around the organs in the pelvis.
-
Stage II or mild endometriosis:
There are more implants than in Stage I but damage to the pelvic organs is still pretty minimal and there’s not much scarring or adhesions. Altogether, when summed up the implants are not more than 5cm (couple of inches).
-
Stage III or moderate endometriosis:
Implants are more widespread and are beginning to infiltrate (grow into or invade) the organs in the pelvic region, including pelvic side walls (where the blood vessels, major nerves and ureters are located) and peritoneum. There is more scarring and adhesions and endometriomas (“chocolate cyts”) of old blood in a blister on the ovary, can be seen.
-
Stage IV or severe endometriosis:
The disease is definitely infiltrating or growing into and affecting several organs in the pelvic region as well as the ovaries. This may be the bladder or the rectum. Anatomy is severely distorted with scars and adhesions and there is fibrosis (like concrete) between organs. Larger and more endometriomas can be seen.
Endometriosis Surgical Treatment
Purpose: Diagnosis and today's gold standard initial treatment (pain relief, infertility, suspicious masses).
Approach: Minimally invasive excision surgery provides accurate diagnosis and effective symptom relief.
Caution: Surgery should be strategically timed, as repeated procedures increase scar tissue and risk.
Balanced Decision: Benefits must always outweigh risks; timing and surgeon expertise are critical for optimal outcomes.


What Type Of Surgeon For Endometriosis?
The type of surgeon needed for endometriosis treatment depends on your specific situation—whether it's initial diagnosis, managing recurring pain, evaluating suspicious pelvic masses, or addressing infertility concerns. Each scenario might require a team of consultants for your individual needs.
What you get with us and why may this be VERY important?
The highest possible surgical expertise based on extensive training far beyond MIGS-level fellowships, an intense focus on endometriosis and related malignancies, internationally vetted and highly respected robotic master surgeon who trains others.
In general, to get a correct diagnosis a general gynecologist can do that but surgical training limits the treatment part in all but the most basic of cases. However, if you are being treated without biopsy proof of endo, get a second opinion with either a reproductive endocrinologist (a subspecialty of ObGyn) or a fellowship trained endometriosis surgeon. If you know you have endo and need an excisional surgery for endometriosis treatment, consider a fellowship-trained gynecologic endo surgeon and/or a gynecologic oncologist. The more the disease is advanced and the more the pelvis is likely to be very scarred and anatomy distorted, a gynecologic oncologist should be involved for the treatment of endometriosis.
Why should a “cancer surgeon”, a gynecologic oncologist, be involved in endometriosis treatment? Because gynecologic oncologists have an advanced skill set to operate not only on gynecologic organs but also on surrounding intestine, rectum, ureters and bladder; all of which can be affected with endometriosis in advanced cases. Also, endometriosis is associated with an increased risk of ovarian cancer as well as degeneration of endometriosis itself to clear cell cancer or sarcoma. These are things you do not want missed and are especially important to be evaluated for as you get older with a diagnosis of endometriosis. Your life is worth at least an opinion about all of this sooner than later from the right expert, a gynecologic oncologist.
If your main concern is about fertility issues with a diagnosis of endometriosis, a reproductive endocrinologist’s opinion would be very helpful. We can help you find the right specialist if we are not the right fit for your needs. We collaborate and work with many general gynecologic surgeons, fellowship-trained excisional surgeons, and reproductive endocrinologists to help you build your team to beat your endo. We also provide integrative holistic support and can guide you in this regard as well.
Laparoscopic Excision
Minimally invasive surgery starts with laparoscopy, or “keyhole” surgery through small incisions instead of a big vertical or horizontal “bikini cut” C-section type of incisions. A camera instrument and operating instruments are inserted through these incisions, which can number from one belly button incision to four or more, depending on how many and what type of instruments are required. The instruments are scissors and graspers that are “straight stick”, which means they can only open and close in one direction. This is reasonable for relatively easy endometriosis surgery excisions but lacks finesse for more difficult surgery with advanced endometriosis and scarring.

The laparoscopic camera usually used is pretty sophisticated and offers good visibility, but in most cases lacks 3-D (three-dimensional) view and is not generally able to be magnified. In some centers, 3-D laparoscopy with magnification is available but not very common. Why is this critically important? It is not possible to predict how bad the endometriosis will be or how much scarring there is or what organs might be involved. So, once again, for basic excisions or biopsies or even basic hysterectomies, it is adequate.
For more advanced surgery losing that 3-D third dimension is like operating with one eye closed. You lose the depth perception that is very important for delicate surgery in difficult spaces. Try closing one eye and doing things around the house. It’s harder to do isn’t it? Picking things up is not as exact. You can certainly compensate, as people do when they lose an eye, but it’s harder to judge what is further from or closer to you. So, given a choice, using both eyes is better and 2-D laparoscopy screens mimic having one eye closed. This is part of why robotic surgery adds safety to endometriosis excision.
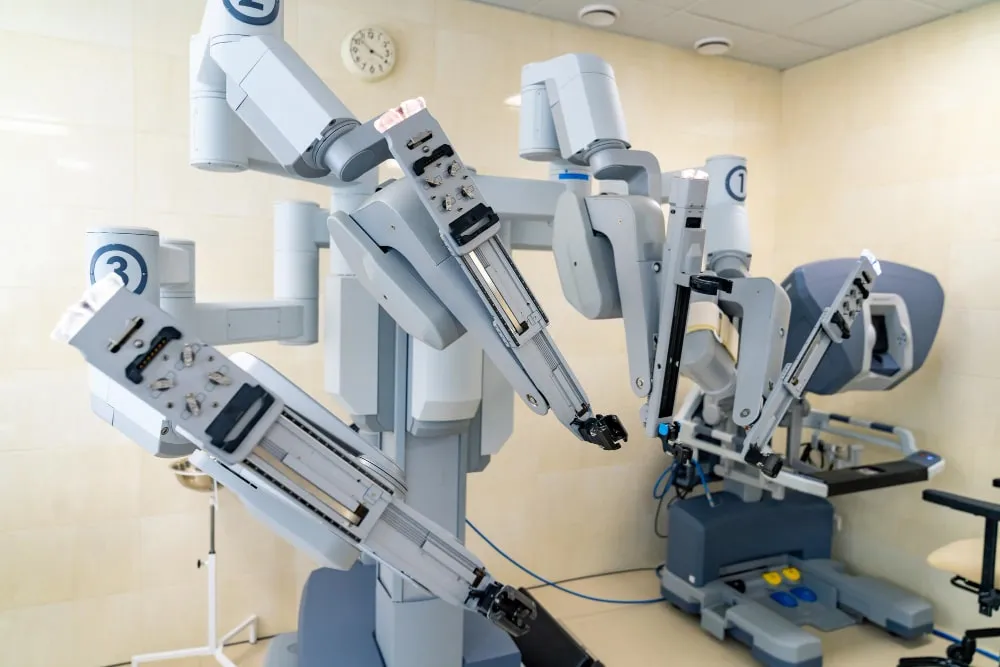
Robotic Surgery Excision
Robotic surgery for treatment of endometriosis by excision is the 21st century tool of choice. It is laparoscopy on steroids, so to speak. While there are expert laparoscopists who argue that robotic surgery does not add anything beyond laparoscopy, the arguments used are usually cost-benefit business-related mumbo jumbo, some of which is only true when centers are not used to using robotics. But this is not your problem anyway because the cost is NOT transferred to you as a patient. You want the best equipment and the best surgeons possible to help you beat endo.
Robotic surgery for treatment of endometriosis has many features and clinical benefits. These are only some of them:
-
Less tissue injury internally due to finesse wristed instruments
-
Less blood loss because of the instruments and better visibility
-
Less trauma to your abdominal wall because the instruments do not move as much
These features lead to:
-
Shorter recovery time
-
Less scarring
-
Fewer complications, transfusions and readmissions
-
Fewer “conversions” to a big incision due to inability to finish the surgery via minimally invasive approach
-
Better ability of surgeon to excise endometriosis
Drawbacks of robotic surgery include a slightly longer time to complete the surgery (mostly the setup time before surgery starts), it is more costly (but your co-pays are the same as laparoscopy), and it is not easy to learn. Many surgeons take robotic surgery training, but you do not want a rookie surgeon for complex endo surgery. Select wisely. We realize some studies are published which still claim no difference compared to laparoscopy. It’s important to realize that studies do not capture all the differences between patients and statistics are complex. Without video proof, it is hard to tell if the surgery was even the same quality and extent. So, as mentioned, laparoscopy is certainly a reasonable tool for many cases but do you want to take a chance that your case may be a bit too difficult for a surgeon with one eye (2-D) and without wrists (straight stick instruments)? As noted, at GOI we approach cases individually but have the robot available for your safety and best outcomes.
Integrative Natural Support
For mild symptoms of endometriosis, there are integrative natural support options to consider and here is an example of some of them:
-
Turmeric:
-
Ginger:
-
Chamomile:
-
Bromelain:
This spice contains a bioactive ingredient called curcumin, which is a strong anti-inflammatory. Pepper helps its absorption. It’s best to use the root or spice and just add to your salads or as part of curry dishes.
This natural root also reduces inflammation and helps reduce nausea that may be caused by the pain of endometriosis. You can make ginger tea by boiling 1 tablespoon of grated ginger into 2 cups of water for 10 minutes. After straining it, add honey. You can also get some ginger pieces and simply chew on them as needed.
This natural herb from daisy-like flowers is also an anti-inflammatory. But beware that it is also a diuretic, so it can make you feel the urge to pee often. You can make chamomile tea by steeping 2 teaspoons of dried chamomile mix in 1 cup of hot water for five minutes, straining it and adding honey for sweetness if desired. Chamomile supplement capsules also exist if it’s inconvenient to make tea.
Bromelain is an enzyme which helps digest protein and has been used as a digestive aid and anti-inflammatory agent. It can be taken in capsule form, but fresh pineapple pulp is a great source.
Endometriosis Treatment Outcomes
Cure Rates
It is difficult to cure any disease when the exact cause is unknown. Such is the case with endometriosis. As we enter the molecular age of targeted therapy, this will change. However, today anyone with endometriosis is likely to see it recur after any medical or surgical therapy. So, the best plan is to make sure the diagnosis is correct, consider removing significant disease with minimally invasive surgery (especially deep infliltrating endo), then focus on ways to minimize estrogen excess in your body. This may include medical treatments listed above or simply being as fit and lean as you can be. Often repeat surgery is required, but you want to limit the number of times this is done to limit scarring from the surgery itself, which can also produce pain. Also, the more surgeries are performed and the more scarring (adhesions) that are potentially created, the more complications are increased. Working with a master surgeon is crucial.


Robotic Surgery Endometriosis Excision Outcomes
Regarding the surgical expertise and outcomes with robotic surgery, from focal to widespread endometriosis, we stand very unique on the West coast. The following information is crucially important in selecting your surgeon.
Basic robotic surgery training and expertise in pelvic surgery is becoming more common for many conditions, including cancer and endometriosis treatment. However, currently, radical robotic multi-quadrant excisional surgery is not standard of care because an advanced skill set for this is not sufficiently prevalent among the majority of surgeons.
This expertise is slowly evolving with a relative handful of committed surgeons practicing nationally with adequate experience, who embrace the technique with strategies and tools to minimize risk of conversion to laparotomy while achieving as close to “complete” R0 or CC0 excision as possible. This “R” and “CC” based scoring is something we use for ovarian cancer when life is on the line, not just pain reduction. But the concept is the same, that being to remove the endometriosis as close to “complete” as possible.
Our surgical experience with complex and re-operative robotic surgery spans over eight years and thus far, the results include low conversion rate of <1% with a high rate of complete CC0 macro-cytoreduction and practically all achieving more than "optimal" cytoreduction status with minimal CC-1 remaining disease (almost microscopic and superficial only). In selecting your surgeon it is critically important to understand the following. While today's imaging with MRI, CT and PET-CT is good for larger disease, it is not even close to being perfect in predicting the extent of disease or distribution. Therefore, the endometriosis distribution can be pan-abdominal and pan-pelvic, and beyond. In other words, it can be anywhere and involving any organ. Literally, ALL possible situations need to be anticipated and prepared for to optimize outcomes with the lowest morbidity (complications), lowest conversion rates to a big incision and to get the best possible resection success. We have the specialized tools and advanced expertise to provide a very unique surgical benefit to you even in very advanced endometriosis situations. As noted, we are not alone nationally in offering über-surgical expertise, but are in a unique position regarding the ability to provide minimally invasive surgical options, even in the face of very advanced disease.
Beyond Life With Endo
Beyond beating endometriosis there is quality of life, which can be equally as important. This is especially true because treatment beyond surgery can extend for a long period of time. To achieve the best quality of life after a diagnosis of endometriosis, a personalized treatment plan is crucial to beat your endo and thrive. In addition, the treatment plan must evolve as time goes on. By focusing on you as an individual, and not just on your disease, we guide you every step of the way. We specialize in helping you plan out the best outcomes possible based not just on your endometriosis but also on your body, mind and spirit.

© Steven Vasilev MD | Gynecologic Oncology. All Rights Reserved 2015-2025.