For complex Endometriosis and Adenomyosis care, visit LotusEndo.com
Gynecologic Oncology Institute is no longer accepting new general gynecologic oncology patients, and refocusing on endo & adeno advanced treatment.
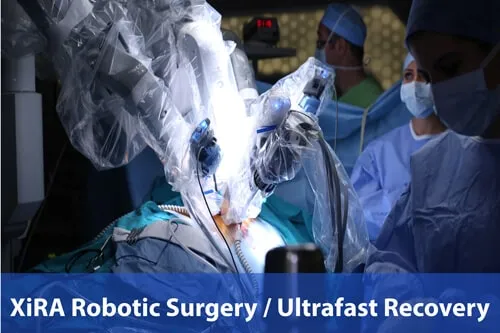
Advanced Surgical Precision for Optimal Outcomes
Experience the Pinnacle of Endometriosis Care with Our Expertise in Robotic Excision Surgery
Endometriosis Excision Surgery
This is the surgical approach of choice at our Center due to superior 3-D optics and wristed instruments, which facilitate as meticulous and precise a surgery as possible. We strongly support this approach over standard laparoscopy with its inherently inferior 2-D “flat” optics and non-flexible instruments. This leads to far fewer complications, excellent outcomes and ultra-fast recovery, even for advanced cases. As a referral center we have performed more complex advanced excision and re-excision surgeries than anyone in the area and accept patients from other states and countries.
Surgical excision of endometriosis is a cornerstone of endometriosis treatment. It is more effective than burning or “fulgurating” endometriosis implants. For the reasons listed on this page, a gynecologic oncologist can be critical to consult with. Dr. Steve Vasilev is a world-renowned expert master surgeon and teacher in complex pelvic surgery. He has taught on the faculty of four major Southern California universities, including UCLA and USC, currently on the Loma Linda faculty. With over 30 years of experience in minimally invasive laparoscopy and robotics, he is an alpha level uber expert for delicate work on the ureters, bowel and bladder and supports endo-excision surgeons in the greater Los Angeles, Santa Monica, Marina del Rey and Beverly Hills areas as needed.
A limited number of patients are accepted directly by application only, focusing on advanced and re-operative endo excision surgery cases and older women with endo and adenomyosis.
Robotic Endometriosis Excision Surgery Or XiREX
This is the surgical approach of choice at our Center due to superior 3-D optics and wristed instruments, which facilitate as meticulous and precise a surgery as possible. We strongly support this approach over standard laparoscopy with its inherently inferior 2-D “flat” optics and non-flexible instruments. This leads to far fewer complications, excellent outcomes and ultra-fast recovery, even for advanced cases. As a referral center we have performed more complex advanced excision and re-excision surgeries than anyone in the area and accept patients from other states and countries.

Endometriosis Diagnosis
Although we are getting closer to bio-molecular testing that might help diagnose endometriosis, the only way to do that today is through surgery and biopsies. In most cases the implants are too flat and small to biopsy with a needle through the skin, even if the radiologist sees something on ultrasound or MRI. So, surgery is the only way to accurately see the lesions and biopsy them and get pathology confirmation.
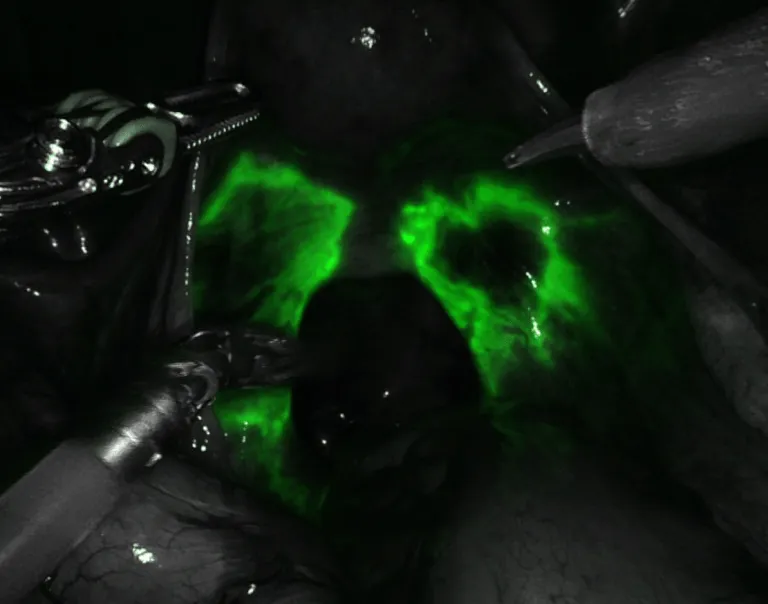
XiREX high tech magnified and 3-D optics allow you to see endo that can be missed through conventional laparoscopy. When you add in Firefly bio-luminescent dye technology to light up the endo, it’s a sure fire bet that if it is there it will be found. This is also useful to make sure bowel and bladder and ureters are viable (good blood supply) if dissection is required on delicate structures. This is an advanced tool, not available everywhere and with published encouraging reports, but it is not standard of practice. However, the point is, in the hands of an experienced and expert surgeon, it is an extra tool that has no side effects or risk and there is no extra cost to you the patient.
Excision of Endometriosis
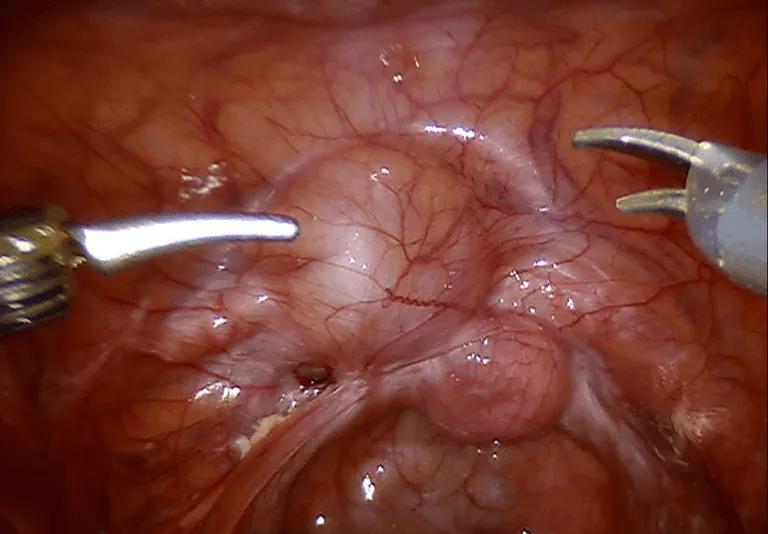
Removing endometriosis, or endometriosis excision surgery, is the second goal of surgical therapy. In most cases the problem areas, which are most commonly in the pelvis, can be removed.
The endometriosis grows on the peritoneum primarily (your internal “skin” lining) and patches of it can be removed or “excised”. Endo can grow on the ovaries, the bowel, the bladder and other organs as well.
The goal is to remove as much as possible. When dealing with delicate structures like the bowel, precision instruments and a highly skilled surgeon are critical to success.
While total pelvic peritoneal excision for endometriosis is not usually possible, a judiciously large amount can be safely and effectively removed. The peritoneum grows back. Since the peritoneum covers literally everything, including the tubes, ovaries and uterus, radical excision means removing the uterus, tubes and ovaries. But this is not required at all for most cases.
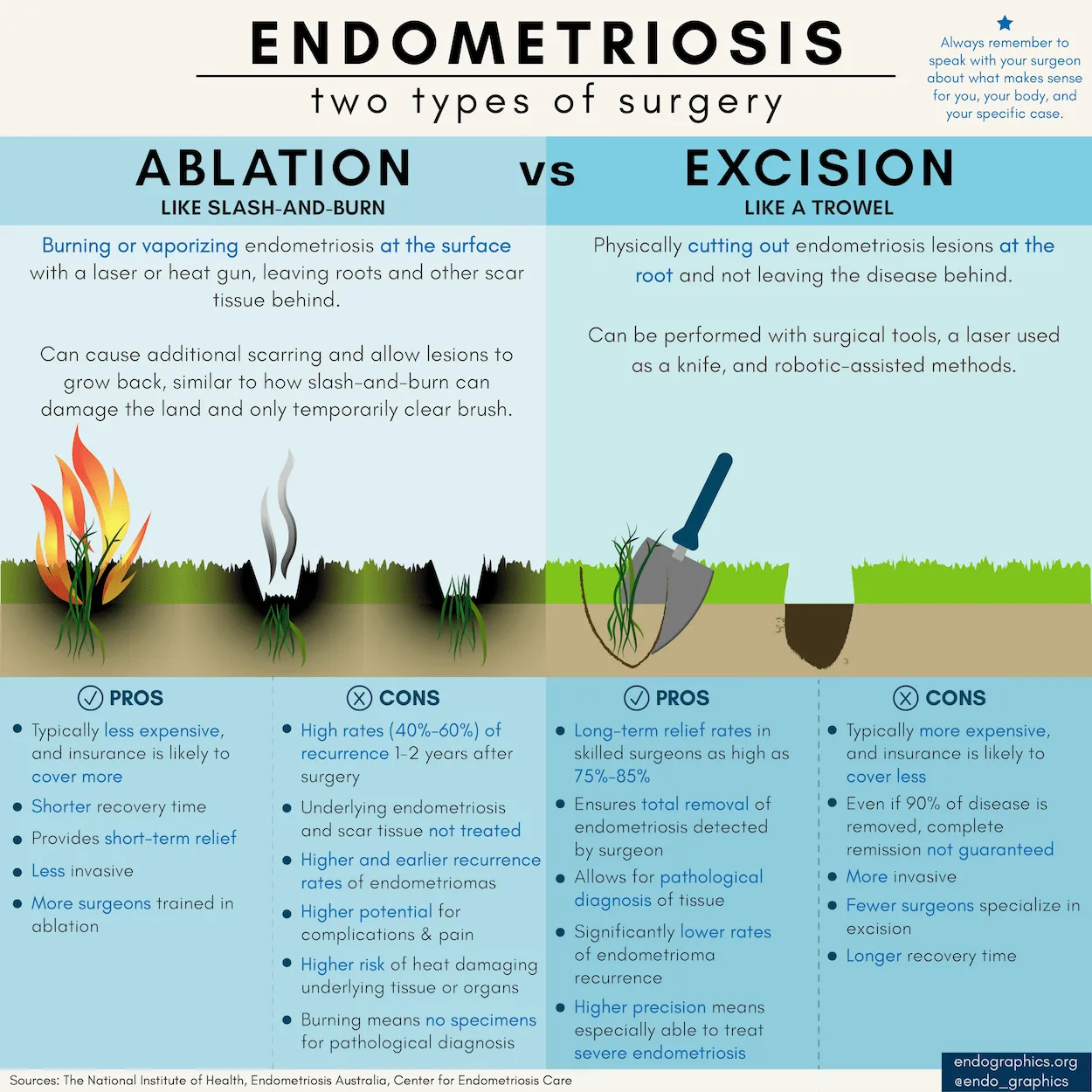
Endometriosis Ablation vs Excision
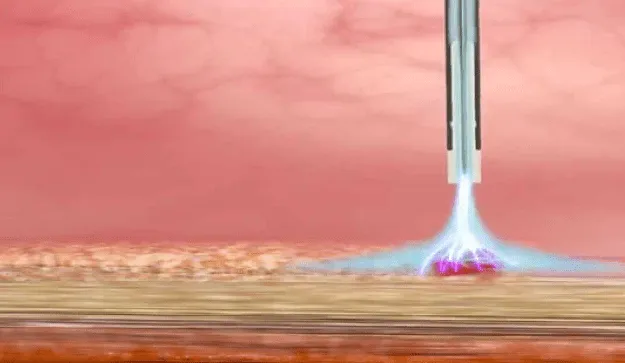
Fulguration or ablation means burning or destroying the endometriosis tissue with something like cautery or laser (laser can cut and ablate). This is still the standard of practice among most gynecologists, even though it is far less reliable in removing the endo. It is less reliable because it is not possible to tell exactly how deep the lesion is and if fulguration is destroying all of it or not. The less it is completely destroyed, the greater the chances it will grow back. Also, the surgeon is only guessing what is endo and what is not. Sometimes it is easy to tell and in other cases it is possible that the surgeon is torching delicate structures for no benefit and potentially injuring organs that lie beneath the peritoneal surface (e.g. the ureters). In addition, it is a well known principle that cautery leads to more scarring than cold scissors excision with judicious cautery for bleeding only. More scarring postoperatively means more healing issues and potentially more pain.
Limited Ablation With Advanced Technologies
Although most of today’s optimal surgery is based on excision, some delicate areas harbor a lot of tiny superficial implants, like the bowel. In this situation, assuming a highly skilled surgeon, more endo can be removed using technology like the Argon Beam coagulator or cold plasma generators to destroy the lesions without having to remove large sections or multiple sections of the bowel. So, there can still be some added benefit to fulguration, in addition to excision of most of the endo, in skilled hands. This requires expert surgeons and the right settings so that the depth of injury is minimized to microns, not millimeters (e.g. the small bowel is only a few millimeters thick in some areas).
Endometriosis Excision Surgery Complexity
Surgery for endometriosis can be relatively simple or very complex and it is extremely hard to predict which it will be, even with the use of high-tech imaging including MRI and ultrasound. In some cases the anatomy is fairly normal and in others it is completely obliterated from the inflammation and scarring that endometriosis causes. If you have had abdominal or pelvic surgery in the past, the adhesions or scars can be even worse. Segments of small and large bowel can be involved as well as the urinary system, including the bladder and ureters (delicate tubules that connect your kidneys to your bladder). Additional pathology like uterine fibroids or adenomyosis can complicate the surgery further, as can related primary bowel inflammatory disease like diverticulosis. Finally, it is estimated that 1% of endometriosis can undergo malignant degeneration (i.e. endo can turn into cancer itself or be associated with ovarian cancer).
All of the above means you should have a surgeon that is capable of handling any eventuality including removal of segments of bowel or urinary system and safely reconstruct these structures. The surgeon should be able to avoid resection like this and be able to understand the balance or what is going to be beneficial and what can be harmful. For example, resection of too many segments of other organs or inadvertent damage to too many segments of bowel can increase the risk of fistula, which means leaking urine or stool or small bowel contents and possible severe infections due to abscess formation. Ideally, no inadvertent damage to organs should occur. However, endometriosis can create scarring almost as firm as concrete and dissection can become very complex. Prudent decision-making during excision is uber important for safe and effective surgery.
In the relatively rare event of cancer found during surgery, the surgeon should be prepared to remove what is necessary and biopsy areas like lymph nodes to make sure cancer has not spread. If it has spread, then removal of all visible disease is even more important than removal of non-cancerous endometriosis implants. Gynecologic oncologists are the surgeons who have the most expertise in safely removing cancer tumors or implants from all involved organs. While a team of gynecologists, endo-excision surgeons, colo-rectal or general surgeons and urologists can often get the job done in endo excision surgery, there is potential for disagreement as to the best overall surgery plan and this is one case where you do not want too many cooks in the kitchen as they say.
The less complex the surgery, the less you need a gynecologic oncologist involved. For the simplest cases an experienced gynecologic surgeon that understands endo is more than adequate. For more intermediate to complex cases a fellowship trained endo-excision surgeon would be a better bet to get the job done safely. The more complex it turns out to be, a gynecologic oncologist becomes almost mandatory.
How do you know before surgery how complex it will be? You don’t! Having said that, if you are older, if you have a family history of cancer, if you have undergone prior abdominal or pelvic surgery, if you have large endometriomas (based on ultrasound or MRI), or you are told that your pelvic exam is very “stuck” or “frozen” (meaning the uterus and ovaries are not moving very much during a pelvic exam), the more likely you will be facing a complex surgery. As mentioned, a gynecology/endo-excision surgeon, combined with general/colo-rectal surgery and/or urology can often handle many such cases. However, hands down, the most experienced “complete” pelvic surgeon for complex pelvic surgery involving the uterus, ovaries, bowel and urinary system, is a gynecologic oncologist. The only downside is that gynecologic oncologists focus on cancer and not all understand the pathogenesis of benign endometriosis. In that case, the best team is a gynecologist oncologist and an endo-excision surgeon.
Personalized High-Tech Surgical Care
Endometriosis is highly variable, so you should seek personalized treatment options. More importantly, just like endo varies, so do individual people and their specific situation.
Treatment options should be based on how early your endo likely is, your fertility goals, the most likely effective treatments, and reducing the risk of recurrence with integrative modalities.
Most important are individual needs not only to survive but also to thrive.

Endometriosis Excision Approaches and Tools
Laparotomy
The relatively old-school approach of making larger incisions, whether vertical or transverse (bikini-cut or like a C-section) is rarely required. However, never say never. Sometimes, this is the only safe approach or is necessary to convert to during surgery if a minimally invasive approach is unsafe or complications, like excessive bleeding, have occurred. In Dr. Vasilev’s hands, the conversion to laparotomy from robotic minimally invasive surgery is almost zero over the last five years.
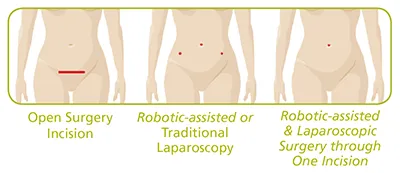

Minimally Invasive Surgery Incisions
Before we compare and contrast the different minimally invasive techniques, keep in mind that where incisions are placed, where some or all of them can be hidden, what the planned surgery is, how large the incisions are (they are all variations of “tiny”), depends on the surgeons, safety and your wishes about body image.
These should all be considered and it is not “one size fits all”.
Instruments range in size and require from 2mm microsurgical to the more commonly used 5mm laparoscopy or 8mm robotic surgery incisions. Some can be a bit larger, as in the single site belly button approach discussed below. They all have different risks and benefits and how many depends on what needs to be done and the surgeon’s skill and experience. On average there are 2 to 4 small incisions, many of which can be hidden in the belly button or below the bikini line, but this is not always the case. Keep in mind that unless you form keloid scars (most don’t), these incisions can all be faded over time with postoperative care approaches using enzyme bandages and various preparations that are friendly to help skin healing.
Laparoscopy
A laparoscope is a narrow (usually 5 millimeters or quarter of an inch) telescope-like instrument, which is approximately 30 centimeters (about 12 inches) long. It is introduced into the abdomen or pelvis through a small incision, usually in or near the belly-button. A light is part of the instrument and it allows the surgeon to see inside your body when the scope is attached to a camera, which transmits the images to a TV screen in the operating room. The surgeon uses that screen in two dimensional view (means there is no depth perception) to see what they are doing. There are a few systems that have surgeons wear 3-D goggles (like those used for video games) which simulate three dimensional surgery, but these are not the norm.
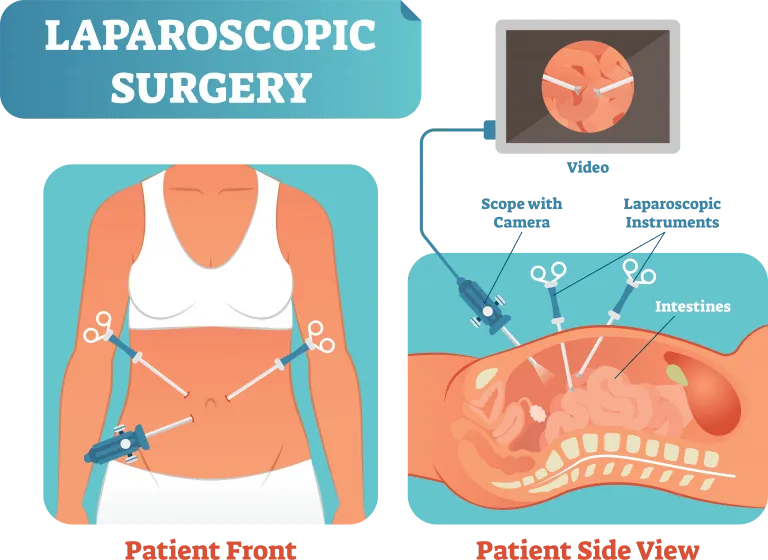
Additional incisions, often one or two, sometimes three or four, usually all small and around 5mm, are used to place operating instruments. These instruments have tips that grasp, cut or cauterize and are straight. In other words, they do not flex or bend. This creates a situation that is reminiscent of doing things with chopsticks, with limited motions limited to cutting, pushing and pulling. In many cases, usually when anatomy is not too distorted, this type of surgery is adequate, “just OK” or good enough to get the job done. With more complex and distorted anatomy, lack of precision can lead to more bleeding and accidental injury. Also, since the fulcrum of the surgery is the abdominal wall (the point at which the instruments are pivoting) the abdominal muscles are pushed and pulled a lot, which means more trauma and more possible pain after surgery. This is still far better than pain from big laparotomy incisions, but is a concern nonetheless.
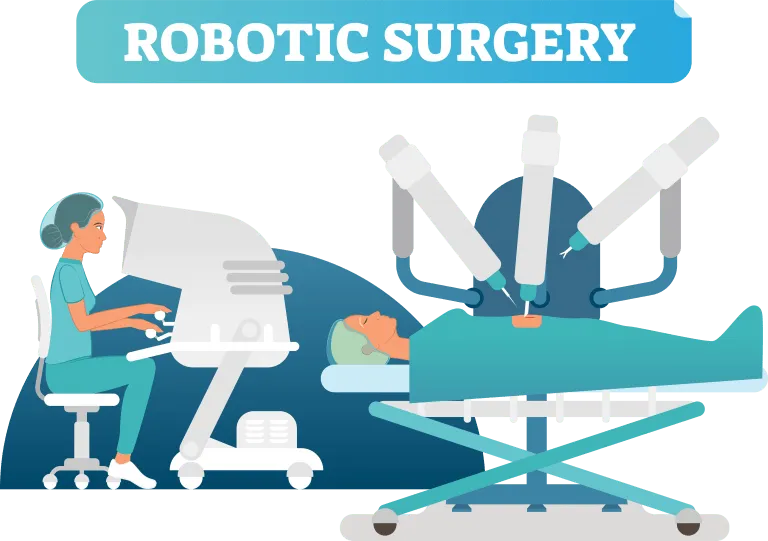
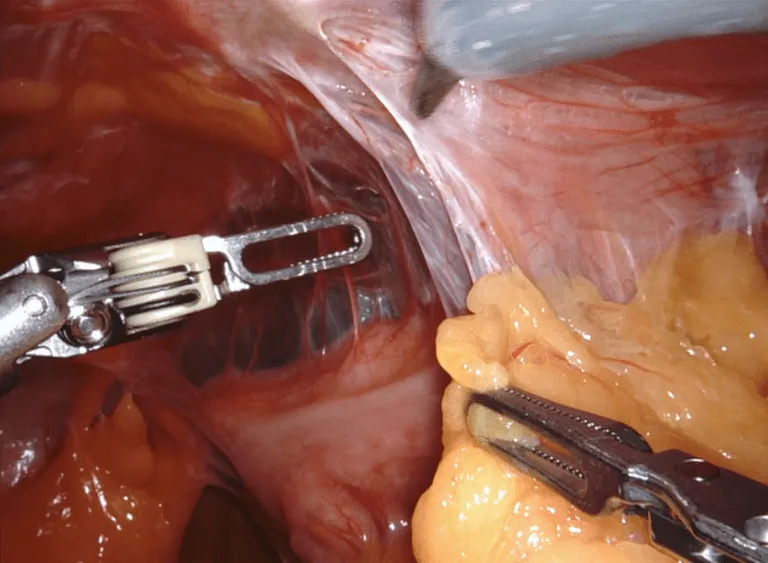
Robotically Assisted Laparoscopy
Robotic Surgery is basically an advanced form of laparoscopy with better and magnified optics in 3-D, better more precise instruments and more control of steady motions. The most commonly available robotic instrumentation is the DaVinci system from Intuitive Surgical. The incisions are a tiny bit larger at 8mm with a minimum of three incisions, one most often hidden in the belly button. In this type of endometriosis excision surgery, the surgeon in at a console a few feet from the patient and 100% controlling the robotic instrument movements. A bedside assistant surgeon helps with placing the instruments as needed.
With either robotics or laparoscopy it is possible to do one belly-button incision through which multiple instruments can be placed (single site surgery). The incision is bigger but curved and hidden in the belly button. The only problem is that deeper (where the muscles are) it cuts enough tissue (1-2 inches) that your risk of a hernia in this very weak area of the body (your belly button) increases substantially from almost zero to approximately 3-4%. This is not a routine approach in our hands because of this, increased infection risk and other technical reasons. Once you have a hernia, they tend to recur. So, one has to think long and hard if it is worth it compared to a couple of tiny incisions that may not be hidden as well, but heal very well in most cases to where you can hardly see them down the line. However, in some cases it might be right for you if you don’t mind the increased risks and possible need for hernia repair surgery down the line.
The camera is high-definition 3-D, and capable of magnification for difficult dissection areas, which means the surgeon can tell how deep one structure is relative to another one (i.e. depth perception) and can avoid injuring structures that are millimeters away from lesions that need to be precisely excised. With magnification, when necessary, it’s like having a microscope available to further enhance accuracy.
This means fewer complications and less bleeding on average, but especially in complex surgeries.
The instruments are “wristed”, which means they move much like a human hand rather than a straight chopstick at the tips, where the surgical action is.
This translates into FAR more precision and stability since the instruments are mechanically stabilized and not allowed to shake or amplify a tremor from the surgeons hands, like what happens with laparoscopy. Meticulous surgery means less trauma at each point and that means better healing.
Also, since the fulcrum of the surgery is NOT at the abdominal wall (i.e. the action is at the wristed instruments at the tip), there is less trauma on the abdominal wall muscles and less resulting pain during recovery..
When the surgery is highly complex, the surgeon actually has three arms to interchangeably control instruments and essentially assist themselves rather than asking the assistant to grasp or hold something and make mistakes due to miscommunication. The assistant then only assists by exchanging instruments into the robotic ports when the surgeon requests a different instrument (e.g. scissors instead of a second grasper), or uses suction when minor bleeding occurs.
What is a DaVinci Robot?
It’s important to realize that the robotic technology only facilitates what the surgeon does. The robot is not able to do anything by itself. Here’s how it works. The robotic arms are positioned over the patient during surgery. There are four arms, three which hold different instruments, and one that holds the 3-D camera. Sometimes all four arms are used with four incisions and sometimes only three are used.
The robotic arms are controlled by a computer that replicates movements made by the surgeon at the surgeon’s console, a few feet away from the patient. The console has a stereoscopic 3-D viewer and the robotic controls, requiring use of both hands and feet to fluidly and gently control instrument motions.
Is Laparoscopy or Robotics “better”?
The biggest beef against robotics is that it “costs more” and “takes longer”.
If you believe the “cost” studies should determine if you get the best treatment, then it is true that robotic technology on average costs more to run. BUT, and this is HUGE, this cost does NOT get transmitted to you as a patient AT ALL! Surgeons are not paid more and hospitals do not charge you or your insurance carrier more. So what’s in it for them you ask? Surgeons are more comfortable using the robot, especially for longer cases, and a calmer less tired surgeon means less complications. Hospitals want happy surgeons to use their facilities. So, there you have it.
In terms of “taking longer”, if the team is not used to working with the robotic equipment, then it might take 10-15 minutes longer to set up. The tradeoff is all of the benefits which may actually make the surgery faster while remaining safer. In a high-volume center, such as ours, there is no time difference at all because the teams are well coordinated.
Benefits Of Robotically Assisted Surgery
-
Less conversion to laparotomy for more difficult cases
-
Less pain because of less trauma from precision instruments
-
Less blood loss due to better optics and instruments
-
Shorter recovery time
-
Less scarring due to less trauma
-
Fewer complications
-
Quicker recovery and return to normal activities due to less abdominal wall discomfort
-
Less need for narcotics for pain after surgery
Selecting incisions for endometriosis excision surgery is up to the surgeon after a discussion about body image and trying to hide some or all of the incisions. So, if it is reasonable, then three 8mm incisions are all that is needed for robotic surgery. It is true that with laparoscopy it is sometimes possible to get easy cases done with only two incisions. Also, laparoscopy uses 5mm incisions and robotics uses 8mm incisions. This difference of 3mm is hardly ever noticeable.
Practical Advice: Deciding on Laparoscopy vs. Robotics
The following mental simulation is why it is our strong opinion that robotics is far better than laparoscopy for most endometriosis excision surgery cases.
Try to visualize this in your mind rather than doing this. But if you do this, PLEASE have someone around to help you so that you don’t injure yourself.
Imagine taping one of your eyes closed with an eye patch. This takes away the 3-D vision that most of us who are blessed with two functioning eyes take for granted in day-to-day living. Now you may notice that it is harder to tell how far things are away from you. You have lost depth perception. This simulates 2-D laparoscopic surgery optics on a flat TV screen (rarely, surgeons may have simulated 3-D available on TV).
The cartoon below makes this seem kind of funny, but having a one-eyed surgeon operate on you is anything but funny! One-eyed or 2-D surgery means no depth perception for detailed work in critical areas, especially with distorted anatomy as is often present with endometriosis.
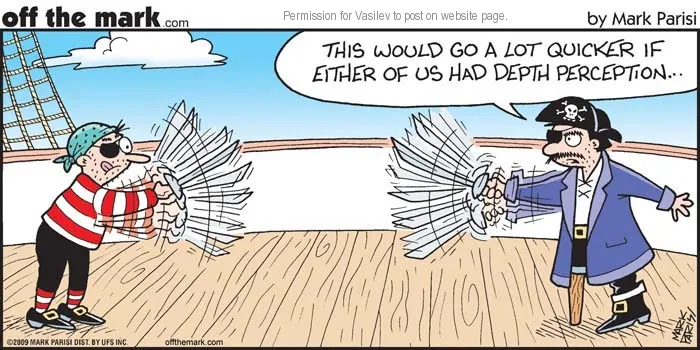
Now imagine taking some tape and splints and making your elbows and wrists immobile. Or, imagine full arm casts on both arms. Then imagine taping all your fingers together except your thumbs and index fingers on each hand. This is what straight-stick laparoscopic instruments are like. You can push, pull, cut, and tear, and if you get good at it maybe few slightly more finesse moves.
With the eye patch and taped arms, wrists, and fingers, imagine going about doing daily activities (please do not drive and do not actually do anything without close assistance).
We are humans, and we can eventually adjust. But why did we evolve with two eyes and arms with elbows, wrists, and versatile wristed hands? Because it is FAR more efficient and safer to have all of this in working order. This is the difference between laparoscopy and robotically-assisted surgery. Simple stuff may be possible, but the more complex harder surgery is more dangerous to accomplish. With laparoscopy, the surgeon is operating in constant “workaround mode” to make up for the deficiencies in the instruments.
Be wary of those who proclaim robotics are “training wheels” for laparoscopy and useless costly gaming-like technology. Is robotics necessary for all surgeries? No. But is it intrinsically “better” because it is 3-D instead of 2-D, magnified instead of not, more finesse wristed instruments vs not? Absolutely!
Read the part about surgical complexity above again. There is no way to know in advance if a simple surgery might actually be simple. At that point, it is prudent to have the very best technology available to the surgeon for all eventualities. Remember, “it’s OK” surgery is not OK and not good enough.
Laparoscopy vs Robotics Head to Head
So, OK, you’re not a grape, but this illustrates the precision robotics motions vs jittery motions of laparoscopy in a very delicate situation. And in this case Mr Grape’s anatomy is actually normal. When NOT normal, the imprecision is amplified. The devil is in the details. Rock steady robotically assisted precision vs. jittery clunky laparoscopic “straight stick” surgery….and this is with an EXPERT surgeon! Imagine how much worse a less skilled set of surgeon’s hands might be.
Possible Excision Surgery Components
Endo excision may mean simply removing some relatively small peritoneal patches which do not involve critical structures like bowel, ureters, rectum, small bowel or even stomach. But in some cases some of these structures are involved or very close nearby. In some cases these implants can be shaved off and in some cases a section of bowel, bladder or ureter may need to be removed and then repaired.
The uterus can be superficially coated with endometriosis implants but usually these can be removed without a hysterectomy.

However, the uterus can be involved with a highly related condition called adenomyosis (internal endometriosis), which can be contributing to pelvic pain and very painful periods with heavy bleeding. If fertility is a concern then the uterus can certainly be left alone. If babies are not in future plans, then excision may include a hysterectomy, which may reduce the risk of repeat surgeries due to persistent pain. This is something to discuss in detail with your surgeon.
The ovaries can be involved with superficial implants and these can be excised or superficially fulgurated if the goal is to preserve as much ovarian tissue as possible. Fulguration is generally not the ideal approach but excision may actually remove more ovarian tissue than pinpoint fulguration, sparingly used. Sometimes endometriomas or chocolate cysts (old dark blood-filled sacs) can be present which can make surgery far more challenging because of more inflammation and scarring. If fertility is no longer desired and the anatomy is heavily destroyed with multiple endometriomas, then one or both ovaries may need to be removed rather than leaving behind endometriosis tissues on the ovaries. These cannot always be easily “peeled out”, even with aqua-dissection (hydro-dissection). Also, if the ovarian mass does not look like an endometrioma and maybe be a tumor (benign or malignant), then removal may be necessary. This again requires a long conversation with your surgeon and presumes the surgeon has a wide and deep skill base and understanding of endometriosis. Presuming this is not a good idea. See below regarding finding vetted surgeons via iCareBetter, which so far (2021) is still a small international group of expert surgeons but will likely grow rapidly.
The Fallopian tubes are very delicate and necessary structures for passing eggs to the uterus during reproduction. If these are heavily damaged they may need to be removed to lower the risk of pregnancy in the tube (ectopic pregnancy), which can lead to heavy bleeding and cannot go to term as a normal pregnancy. For these decisions you may want to involve a reproductive endocrinologist, weighing the risks of keeping damaged tubes in vs assisted reproduction like IVF.

The appendix can be involved and it may be prudent to remove it because it can harbor endometriosis, can harbor other pathology including cancer that may be more common with endo, and for prevention of appendicitis. This depends on your age and on the surgical findings, but is something to discuss with your surgeon before surgery. The risk is low, but is not zero, and mostly related to possible bowel leak and infection.
Rarely, nerve ablation or removal is recommended. These procedures include presacral neurectomy and laparoscopic uterine nerve ablation (LUNA). These are being advised less often because they are not uniformly successful and can interfere with rectal and bladder function, forever. If pain is severe, and a temporary nerve block (using needles) is effective, and it does not cause untoward bladder or bowel dysfunction, then surgery may be the answer for you. This does not require a neurosurgeon, but is does require a very experienced surgeon because bleeding can be severe in these areas.
Selecting a Surgeon and Team
The hardest decision is usually NOT whether or not to undergo surgery. If you do now know, but symptoms are highly suggestive of endometriosis, then the only way to find out is surgery. If you know you have endo and the pain is becoming unbearable, possibly after multiple surgeries, then repeat surgery may be the only path to pain relief for some period of time. We know endo can recur, but time between recurrences or the chances of recurrence depends at least in part on the quality of excision. Sometimes the biology of the endo is more or less aggressive and surgery can help but not be the final answer and requires medical therapy as well. But the decision to consider surgery can be relatively straightforward after considering the options.

Instead, the hardest decision is often determining who your surgeon and endo treatment team should be. Unfortunately, many women are not aware of options and go with general gynecologists who often are not up to speed on the intricacies of optimal endo management and may not be that skilled in complex surgery.
It bears repeating that one NEVER knows how complex the surgery might be when you get there and look inside. So your surgeon and team should be ready to tackle anything they find…anything! Although repeat surgeries are common when endo recurs, an optimal surgery can reduce that risk.
So, who should your main endometriosis excision surgeon be and how do you find them?
In your search, you may ask friends who have gone through this before, you may ask your primary doctor, you may search online, look in phone directories or even use online educational resources like Nancy’s Nook or other endometriosis groups on Facebook or other social media. Unfortunately, ALL of these options leave a LOT to be desired. How nice a surgeon might be does not mean they are a great surgeon or if they understand endo. Directories are a shot in the dark because everyone is the world’s greatest surgeon if you believe what is written in the ads or on their websites.
An educational resource called Nancy’s Nook is very helpful. Included is a social media sharing of experiences and the site is led by someone who has a personal mission to get quality information out, as in the case of Nancy Petersen and her Facebook group team. There is also an associated website at NancysNookEndo.com. However, even in this helpful medium, “Nook Surgeons” are largely listed based on feedback from patients, who are usually not medical personnel and can’t really tell who is good or not from a technical point of view. Having said that, at least there is a significant basis for the recommendations based on reported patient clinical outcomes. So, what else can one do?
A brand new resource is an organization that vets surgeons internationally based on peer review of video for technical expertise assessment. This organization called iCareBEtter and is growing to include more surgeons to help the millions of women who need vetted expertise in order to avoid botched surgeries and continued suffering. Some combination of the following types of surgeons should be considered.
General Gynecologist
Board certified or board eligible (completed ACGME approved training but waiting for testing certification) gynecologists have been trained over four years to generally diagnose and care for endometriosis. However, this is not a focus of the four year residency training program. Most gynecologists are capable to handling basic surgery but in most cases are not trained to perform extensive excisional surgery, favoring fulguration with cautery or laser instead. Having said that, some have focused on endometriosis treatment after residency and can handle at least diagnosis and basic surgery. The general gynecology mainstream viewpoint is strongly focused on medical therapy of endometriosis, including use and potential abuse of medications like Lupron and Orlissa, which reduce estrogen production. Unfortunately, it is generally argued that general gynecologists get the least intensive surgical training (4 years of both obstetrics and gynecologic surgery) when compared to their general surgery or urologic colleagues (5-7 years of only surgery).


Reproductive Endocrinologist (REI)
This is a sub-specialty of Obstetrics & Gynecology which focuses on reproduction issues and endocrinology, and requires a 18-36 month ACGME approved fellowship to secure additional board certification. They mainly focus on assisted reproductive technologists like IVF. This subspecialty has moved away from micro-surgery and has become more medically based along with very specialized invasive techniques to harvest eggs and so on. If fertility is an issue for you, you should seek a consult from an REI but they will not likely be your best bet for endometriosis excision.
Endo-excision Surgeons
Gynecologists who have sought additional training in endometriosis management enter a non-ACGME approved fellowship that focuses on minimally invasive surgery and endometriosis excision. These fellowships are usually one to two years in duration, and are managed via societies like the AAGL and SLS or are free-standing (like a private apprenticeship). The advantage of this is at least there is additional training. The disadvantage is that the quality oversight is not as strict as ACGME programs and the experience is not as uniform. But there are no ACGME approved endo excision fellowships, so this is as good as it gets at the moment. In general, this additional training clearly produces surgeons who are usually a level above most general gynecologists. Most endo-excision surgeons do not get significant additional training in extensive bowel or urinary tract surgery. This is very variable, and some do. There are exceptions and more gyn trained surgeons in countries outside the USA are variably comfortable with surgery that extends to the bowel, bladder or ureters.


General Surgeons, Colorectal Surgeons, Urologists
These surgeons are not endometriosis excision surgeons. They have undergone 5-7 year ACGME accredited residencies and are board certified or board eligible surgeons that deal with intestinal or urologic conditions as well as hernias and other conditions. However, none are trained in any gynecologic surgery. They are asked to assist in portions of endometriosis excision surgery by gynecologists or endo-excision surgeons when urologic organs or bowel is involved. The problem is that they don’t intuitively know what they need to do for endometriosis. Therefore, they are usually purely a technician to help the gyn focused surgeon. In some cases they have done this for a number of cases as a team-member and become more familiar with what is needed. Until that collaboration is established over time, there can be disagreement as to what procedures should be done between the specialists during surgery.
Gynecologic Oncologists
Surgeons who follow this path have completed a four year ACGME accredited residency in ObGyn and an additional three to four years of ACGME accredited fellowship training in advanced pelvic surgery and complex care of cancer patients. After seven to eight years of training the surgical expertise far exceeds most other pelvic surgeons in any speciality and certainly in gynecology focused surgery. Training includes resection of most organs outside the reproductive tract (uterus, tubes and ovaries) that may be involved with gynecologic pathology, like ovarian and other cancers. This means gynecologic oncologists perform bowel surgery, urinary tract surgery, reconstructive surgery, throughout the abdomen and pelvis.

Resection of advanced ovarian cancer may also include removal of parts of the liver, diaphragm, abdominal wall including muscle, spleen removal, etc to get the cancer out. This serves as uber training to remove endometriosis, which spreads much like ovarian cancer and is almost always invasive (more difficult to remove). Since gynecologic oncologist are cancer experts, they are also able to address those situations when endo goes bad and is associated with cancer (about 1% or less of the time, and most often in older patients).
Finally, the vast majority of gynecologic oncologists have now been trained in minimally invasive surgery, including laparoscopy and robotic surgery. For most gynecologic cancers, minimally invasive surgery is now the standard of practice wherever it is possible. In some cases it is not the best option, but in most cases it is at least a consideration, even for advanced cancers.
Some gynecologic oncologists have focused on endometriosis excision and are known leaders in endometriosis management, while others have not. This variable involvement in endo means that in some cases a gynecologic oncologist is the best surgeon for you (period), since they can handle almost anything that can be encountered. Others are more comfortable working with endo-excision surgeons or gynecologists as part of a team because endo management, as opposed to cancer, is not a significant focus of their practice. At our center, Dr. Steven Vasilev MD focuses on complex surgery including cancer and advanced endometriosis.
Choose Your Surgeon Well : Just OK is NOT OK!
We do not endorse and are not affiliated with AT&T in any way…..but we LOVE this commercial they have. When it comes to your surgeon, just OK is definitely not OK!…whether you are a woman or a man.
Support Team for Endo-Excision Surgery
Pain Management
Most of the time, minimally invasive surgery means less pain during recovery. Often narcotics are not required.
However, if you are already on pain medications, including narcotics, before surgery then managing pain after surgery may include narcotics as well.
For this, a pain management specialist, or an anesthesiologist who specializes in pain, may be very helpful as part of the team.


Pelvic Floor Physical Therapy
Physical therapists who specialize in pelvic floor dysfunction and endo can help both pre and post surgery. This may include manual therapy involving trigger points and visceral manipulation.
Integrative Medicine
As is the case for any other disease, mainstream Western therapy for endometriosis can be complemented by holistic integrative support, some of which is Eastern based or related to the biology of nutrition, microbiome and mind-body relationships. There is a lot of BS being sold out there, but scientific evidence-supported integrative medicine approaches includes acupuncture and acupressure, targeted herbals, a strong micro and macro molecular nutrition program, biofeedback and even some forms of energy medicine.

© Steven Vasilev MD | Gynecologic Oncology. All Rights Reserved 2015-2025.